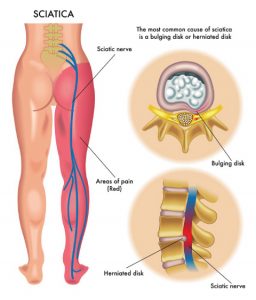
Sciatica is the term used to describe pain felt along the course of the sciatic nerve. The sciatic nerve is the longest nerve in the body. It travels from your lower back through the buttock, and down into the hamstrings and lower leg.
The symptoms of sciatica can include one or more of the following:
- Pain in the buttock and/or leg that may be worse when sitting or standing; it usually only affects one side
- Pain may radiate down the back of the thigh, back and outside of the calf, foot and toes
- Associated tightness and spasm in the surrounding muscles
- Burning or tingling in the leg or foot
- ‘Pins and needles’, numbness, weakness or difficulty moving the affected leg or foot
- Sharp / shooting pain that may make it difficult to stand up or walk
Causes of sciatica:
- Sciatic pain is usually caused by direct compression or irritation of the sciatic nerve, or the smaller nerve roots that form it. This can be due to:
-
- Injury to the intervertebral disc, causing it to bulge or herniate, which can lead to direct pressure on the nerves as they exit the spine (usually the L5/S1 nerve root is involved).
- Degeneration / arthritic changes in the spine, which can lead to decreased disc height, narrowing of spaces between the vertebrae, and decreased space inside the spinal canal.
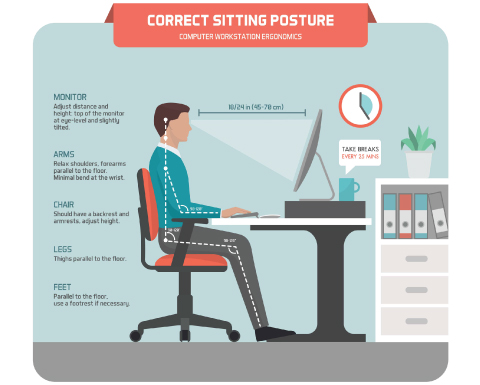
- Restricted or abnormal movement through the lumbar spine due to poor posture, trauma, a sedentary lifestyle and repetitive heavy lifting or loading can lead to irritation of the joints between the vertebrae, inflammation and associated muscle spasm and tightness. These changes can result in irritation of the sciatic nerve.
- Piriformis syndrome – the piriformis muscle is located deep in the buttock. The sciatic nerve runs below or through the piriformis muscle, and tightness or spasm here can irritate the sciatic nerve. It is rare, however, for a tight piriformis to be the only cause of sciatica.
- Sacroiliac joint (S.I.J.) dysfunction – this joint is located between the sacrum and the pelvis. The sciatic nerve runs close to the sacroiliac joint, and damage or inflammation of the joint can lead to irritation of the sciatic nerve.
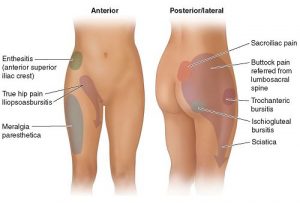
- Referred pain from muscles or joints in the lower back, pelvis or hips can mimic sciatica. Referred pain is usually dull and achy in nature, not sharp or shooting, and it does not usually cause neurological symptoms i.e. numbness, tingling or muscle weakness in the affected leg or foot.
Physiotherapy management of sciatica:
- Most cases of sciatica can be resolved within 6-12 weeks, though this will vary for each individual and is dependant on the underlying cause and severity of the symptoms.
- Your physiotherapist will start by getting a history of your pain and symptoms, as well as identifying aggravating and relieving factors, to help diagnose the cause of your sciatica.
- A thorough functional assessment will then be undertaken, which may include an assessment of your posture, spinal range of motion, muscle strength, balance, sensation and reflexes.
- If further investigation is needed, your physiotherapist or doctor may refer you to imaging of the spine – a CT scan or an MRI.
- The initial aim of treatment is to reduce the irritation of the nerve and to manage pain and inflammation. Your physiotherapist will also advise you to avoid aggravating activities, such as prolonged sitting, bending or lifting. You will start with some gentle exercises to help to reduce your symptoms.
- Once the acute pain and inflammation have settled, your physiotherapist will focus on restoring normal range of motion, flexibility and posture. You will be given an individualised exercise program to address the underlying cause of your sciatica. The exercises will help to correct any muscle imbalances, increase your core control and improve the stability around your lower back and pelvis.
- The aim of the next stage of rehabilitation will be to safely return you to full function in your daily activities and/or sport. Sciatica can recur, mainly due to insufficient rehabilitation. Your physiotherapist will teach you self-management techniques to prevent recurrence of symptoms.
_ _ _
Book an appointment with a physiotherapist today on 07 3358 3915 or info@thebodyrefinery.com.au
Follow us on Facebook, Instagram and Twitter for a daily dose of Pilates and Wellbeing.