The birth of a new child is a joyous occasion that sees many families happily adjust their lives to prioritise their newest addition. But while the focus generally remains on the newborn, it is crucial not to overlook the care required for the mother. According to the Australian Institute of Health and Welfare, 80% of women who gave birth accessed antenatal care throughout the first trimester of their pregnancy. However, there is a lack of records for the later stages of pregnancy and during the postpartum period, suggesting that postpartum care is often overlooked. After nine months of physical, emotional, and hormonal changes, a woman’s body and mind go through a significant transformation that continues to affect them post-childbirth. Therefore, providing proper postpartum care is of utmost importance to ensure the well-being and recovery of the mother.
Postpartum care is not limited to medical check-ups but must be done consistently at home, too. As such, below are some postpartum home care tips to ensure the smooth recovery of any mother.
Take a break from household work
Focusing on their recovery and establishing a bond with their newborn baby is essential during the postpartum period, and this necessitates a break from household work. During recovery, the new mum’s partner and other family members can help share the burden of household responsibilities such as cooking and cleaning. This division of tasks will help prevent the mother from feeling overwhelmed and exhausted. Aside from asking for human assistance, domestic service robots might be another tool to consider. These types of robots help with home maintenance and running errands. With a built-in semi-automated or fully-automated control system, they are designed to perform manual labour and are used for strenuous, menial, or repetitive tasks that can easily be accomplished by technology. Utilising these robots, such as Roombas and Neatos, can greatly help alleviate the strain on postpartum women and reduce the risk of injury.

Seek support from other mothers
One of the greatest advantages of seeking support from other mothers during the postpartum period is the opportunity to exchange experiences and gain valuable insights. With each mother having a unique journey, hearing stories and perspectives from others can offer a wealth of knowledge. This can be invaluable in helping new mothers navigate uncharted waters.
Through local or online support groups such as MumSpace, mothers can have discussions regarding breastfeeding, sleeping patterns, and coping with feelings of being tired. Engaging in such conversations creates a safe space to express concerns, fears, and frustrations without the fear of judgment or criticism. In addition, support from other mothers allows new mums to find solace in knowing that their feelings are valid and shared by others. Empathy from fellow mothers can do wonders in alleviating feelings of isolation and lowering the chance of them experiencing postpartum depression.
Take up some exercise routines
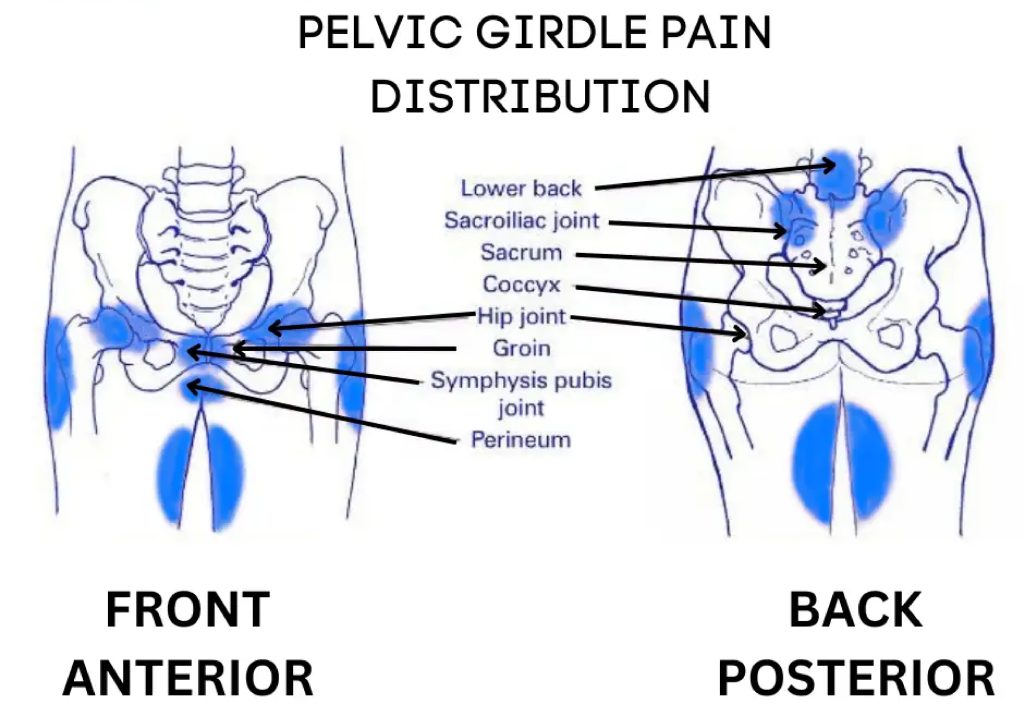
The postpartum period is a crucial time for a woman’s recovery and well-being. Among the various measures to enhance postpartum care, a personalised home exercise program is an effective way to restore pelvic strength and function, especially for those dealing with pelvic girdle pain. These exercises offer numerous benefits, including improved bladder control, prevention of pelvic organ prolapse, and enhanced sexual satisfaction.
The Body Refinery offers various Women’s Health appointments with our Physiotherapists and Exercise Physiologists as well as postnatal classes to help new mums rebuild their strength and confidence.
Article contributed by Ruth Jentson