The Achilles tendon is the largest and strongest tendon in the human body. However, it is prone to injury, with Achilles Tendinopathy being one of the most common overuse injuries.
How does it occur?
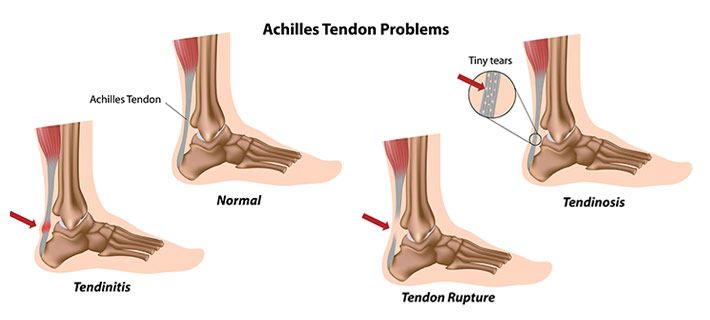
It was previously thought that Achilles pain was due to inflammation. However, recent studies show that Achilles Tendinopathy involves little or no inflammation. We now understand that Achilles Tendinopathy occurs when the Achilles tendon is overloaded, either in a single episode or gradually over time. It has been described as a continuum with three phases: reactive tendinopathy; tendon disrepair; and degenerative tendinopathy.
Reactive tendinopathy is usually seen in younger people and results from an acute overload such as a burst of unaccustomed physical activity or a direct blow to the tendon. In response, the tendon thickens but if the load is reduced, the tendon will return to normal. If the tendon is not allowed to rest however, it will progress to the next phase – tendon disrepair. In this stage, the collagen fibres that make up the tendon become disorganised but it is still possible to reverse these changes with treatment. Things become more difficult in the final stage – degenerative tendinopathy. This stage generally affects middle-aged, recreational athletes who have a history of Achilles pain. At this stage, there are degenerative changes in the tendon that are difficult to reverse.
What are the symptoms?
People with Achilles tendinopathy will report pain, stiffness and swelling in the Achilles region. There are two types of Achilles tendinopathy depending on the location of pain– mid portion and insertional Achilles tendinopathy. Pain in the middle region of the Achilles tendon is typical of midportion Achilles tendinopathy whereas pain, where the Achilles inserts onto the heel bone, suggests insertional tendinopathy.
What are the risk factors?
There are certain factors that can increase the likelihood of developing Achilles tendinopathy. These include:
- male sex
- age >30
- diabetes
- high BMI
- calf weakness and/or tightness
- foot/ankle stiffness.
Other common causes of Achilles tendinopathy include:
- change of footwear
- poor, unsupportive footwear
- change of training surface (e.g. grass to road)
- increase inactivity
How is it managed?
Physiotherapy is highly effective for the management of Achilles tendinopathy. Your physiotherapist will usually provide advice about reducing the load on the tendon and use manual therapy, massage and taping techniques to help relieve your pain. They will also prescribe a specific type of exercise called eccentric exercise. With eccentric exercise, the muscle is lengthening as it contracts. For example, when you do a calf raise over a step. Eccentric training has been shown to not only reduce pain but also improve the structure of the tendon.
Shockwave
If you experience ongoing Achilles pain despite these treatments, please talk to your physiotherapist about shockwave therapy.
Shockwave therapy has been investigated as a potential adjunct to physiotherapy treatment. Studies have shown that shockwave can help to improve pain and function in people with Achilles tendinopathy, especially if it is combined with eccentric exercise. Shockwave uses an acoustic wave which increases blood flow to the injured tendon and stimulates healing.
The Body Refinery’s shockwave machine is made by EMS Swiss DolarClast, the world leader in Shockwave therapy and technology.
The initial appointment is 45 minutes long and will include a full assessment and a minimum of 15 minutes of treatment. Following sessions can go from 15 to 60 minutes depending on the type of injury. Shockwave appointments are only performed once a week to allow the injured area to rest.
_ _ _
Book today to experience the benefits of Shockwave Therapy. Call 07 3358 3915 or follow the link below.
Follow us on Facebook, Instagram for a daily dose of Pilates and Wellbeing.