Rehabilitation for Every Stage: How Physiotherapists and Exercise Physiologists Work Together for Better Long-Term Outcomes
Rehabilitation isn’t a one-size-fits-all process. Our bodies move, heal, and adapt in different ways depending on the type and stage of injury, our health history, and our goals. The Body Refinery combines the strengths of both Physiotherapy and Exercise Physiology to deliver a comprehensive approach to recovery – from the first days after an injury to the long-term management of chronic conditions.
Physiotherapists and Exercise Physiologists bring different, though complementary skills to your rehabilitation journey. When they work together, clients receive a seamless, evidence-based pathway from acute care to long-term strength, confidence, and function.
Physiotherapy: Support for Acute Injuries and Early-Stage Rehabilitation
Physiotherapy plays a central role in the immediate stages following an injury, surgery, or flare-up of pain. During this early period, the priority is to:
- reduce pain and inflammation
- restore mobility and joint movement
- protect healing tissues
- identify contributing factors
- guide safe, early loading and movement
Physiotherapists use a combination of hands-on treatment, targeted exercises, movement retraining, and pain education to support recovery. This stage is crucial – early guidance helps prevent compensations, recurring flare-ups, and long-term dysfunction.
Common conditions Physiotherapists address include:
- acute back or neck pain
- sports injuries
- post-surgical rehabilitation
- tendon or ligament injuries
- acute pelvic, hip, or spinal pain
- pregnancy-related pain
Once pain is better controlled and movement becomes more comfortable, clients are often ready to transition into the next phase – rebuilding strength, capacity, and resilience.
Exercise Physiology: Long-Term Management, Strength, and Prevention
Exercise Physiologists specialise in exercise-based rehabilitation for chronic, complex, or long-term conditions. While physiotherapy focuses on acute injury management, exercise physiology excels in helping clients restore strength, improve physical capacity, and prevent future issues.
EPs are uniquely trained to work with:
- chronic musculoskeletal pain
- osteoporosis and osteopenia
- cardiovascular disease
- metabolic conditions
- mental health concerns
- long-term mobility limitations
- pre- and post-surgical conditioning
- return to sport or return to work programs
This stage of rehabilitation is vital for long-term results. Ongoing, progressive exercise helps:
- improve strength and endurance
- restore movement confidence
- reduce recurrence of injury
- build bone and muscle mass
- support weight and metabolic health
- enhance overall wellbeing and function
Exercise Physiologists also provide tailored programming, education, and coaching to help clients build sustainable, healthy habits.
Why a Combined Approach Works Best
Rehabilitation is most effective when clients move seamlessly between acute care and long-term management. The Physiotherapists and Exercise Physiologists at The Body Refinery regularly communicate about your goals, symptoms, and progress. This ensures consistency and prevents there being any gaps in your care.
A typical pathway might look like:
- Physiotherapy in the early stages to reduce pain and restore foundational movement.
- Exercise Physiology to progressively rebuild strength, mobility, and confidence.
- Ongoing support through Pilates, clinical exercise, small-group conditioning, or specialised programs such as PD Warrior and ONERO®
This team-based model ensures that no matter where you are in your recovery, you’re supported by the right professional at the right time.
Who Can Benefit?
This combined rehabilitation approach is ideal for:
- people recovering from injury or surgery
- individuals seeking long-term management of chronic pain
- older adults wanting to maintain mobility and strength
- anyone needing safe, tailored exercise support
- athletes returning to sport
- those wanting structured, guided movement to stay active for life
Take the Next Step in Your Rehabilitation
Whether you’re at the beginning of an injury or looking to build long-term strength and resilience, our team is here to guide your recovery every step of the way. With Physiotherapists and Exercise Physiologists working together under one roof, you’ll receive a truly comprehensive and personalised rehabilitation experience, with further options including Remedial Massage, Pilates, and Infrared Sauna also available.
Book a Physiotherapy assessment or Exercise Physiology session at The Body Refinery and start your pathway to better movement today.
_ _ _
References
- Booth, J., Moseley, G. L., Schiltenwolf, M., Cashin, A., & Davies, M. (2017). Exercise for Chronic Pain: Effective and Essential. Pain Reports.
- Hopper, C., et al. (2020). Exercise-Based Rehabilitation and Its Role in Chronic Musculoskeletal Conditions.Journal of Orthopaedic & Sports Physical Therapy.
- American College of Sports Medicine (ACSM). (2021). ACSM Guidelines for Exercise Testing and Prescription.
- Bennell, K. L., & Hinman, R. S. (2011). A Review of the Clinical Evidence for Exercise in Osteoarthritis. Best Practice & Research Clinical Rheumatology.














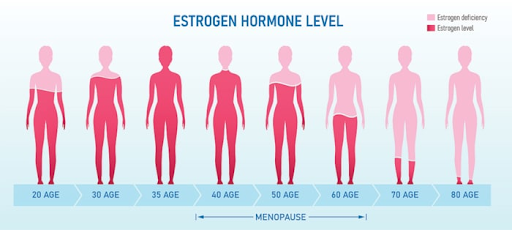 Figure 1. Menopause & the Musculoskeletal System. Sydney Pelvic Clinic, 2025.14
Figure 1. Menopause & the Musculoskeletal System. Sydney Pelvic Clinic, 2025.14