The Facts:
- Menopause onset is defined as 12 months without a period (1)
- The onset is usually between the ages of 45-55, but early menopause can begin in the early 40’s (1)
- Women spend more than one-third of their life in a stage of menopause (perimenopause – post menopause) (2)
How is Musculoskeletal Health Impacted?
Muscular system:
Due to reduced oestrogen levels, women experience an accelerated decrease in skeletal muscle mass, with evidence demonstrating losses of up to 1.5% per year during menopause (3). This reduced skeletal muscle strength can contribute to increased joint pain, reduced functional capacity and greater falls risk. There is also an associated increase in fat mass, increasing cardiometabolic risk and joint loads.
Skeletal system:
Postmenopausal women may lose up to 20% of their bone mineral density in the initial 7 years following menopause due to decreased circulating oestrogen (4, 5). This results in a much higher risk of osteopenia, osteoporosis and fragility fractures, which can in turn lead to chronic pain, loss of independence and increased mortality.
Connective tissues:
Hormonal changes during menopause also affect the body’s connective tissues, with over 70% of women experiencing symptoms.6 Tendons and ligaments become more prone to stiffness, micro tears and injury (7) and have reduced capacity for healing and repair (8). This can manifest as joint pain and stiffness, commonly around the hip, knee, shoulder and ankle. Often, these symptoms impact physical activity levels and recreation.
The GOOD news… there are many ways that you can prevent or reduce your risk of many of these musculoskeletal changes…
5 Key Strategies to Maximise Your Health
- Resistance training – aim for 2 sessions per week. Critical for maintaining (and improving) muscle strength, bone mass, posture and balance, as well as being important for joint and tendon health (9).
- Optimal nutrition – key nutrients include calcium and Vitamin D (bone health), protein (muscle repair) and omega-3’s (reduce inflammation) (10).
- Menopause Hormone Therapy (MHT) – consult your GP or specialist for suitability, may be useful for symptom management as well as bone and muscle health (11).
- Daily exercise – light activities such as walking, yoga, Pilates, swimming and gardening can help with joint stiffness, weight management and mood (12).
- Sleep and stress – mindfulness, sleep hygiene and relaxation strategies can be helpful in reducing pain severity and inflammation (13)
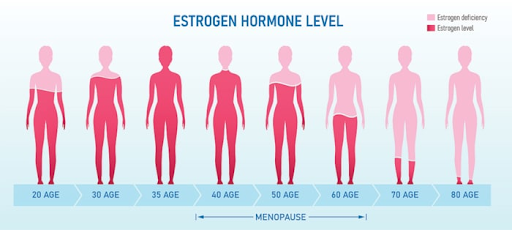 Figure 1. Menopause & the Musculoskeletal System. Sydney Pelvic Clinic, 2025.14
Figure 1. Menopause & the Musculoskeletal System. Sydney Pelvic Clinic, 2025.14
Physiotherapists are well placed to guide you through this critical stage of life, from early intervention and prevention to injury rehabilitation and maintenance programs.
Proactive individual assessments, tailored exercise programs and education are all essential parts of preserving musculoskeletal health, reducing falls risk and empowering women to maintain independence and quality of life.
The Body Refinery’s Physiotherapists and Exercise Physiologists are highly skilled in the area of Women’s Health through the life stages. To book an appointment to discuss how different treatments and/or exercise routines can help you live better, call our friendly admin team on 3358 3915.
Written by Vanessa Alvaro, APA Titled Sports & Exercise Physiotherapist.
_ _ _ _ _
References
1. Turner, K., Crampton, J.S. & Dobbin, N. (2025). Physiotherapists’ perceptions on the management of musculoskeletal conditions in women of perimenopausal and menopausal age: a qualitative focus group study. Physiotherapy Theory and Practice, pp.1-14.
2. Rostami-Moez, M., Masoumi, S.Z., Otogara, M., Farahani, F., Alimohammadi; Oshvandi, K. (2023). Examining the health-related needs of females during menopause: A systematic review study. Journal of Menopausal Medicine, 29(1), p.1.
3. El Khoudary, SR, Aggarwal, B, Beckie, TM, et al (2020). Menopause transition and cardiovascular risk: Implications for timing of early prevention: A scientific statement from the American Heart Association. Journal of the American Heart Association, 9(9), e013219.
4.> National Institutes of Health (2023). Osteoporosis and Related Bone Diseases National Resource Centre. Retrieved from: https://www.bones.nih.gov
5. Greendale, GA & Sowers, MF (1997). Bone mineral density loss in relation to the final menstrual period in a multiethnic cohort: Results from the Study of Women’s Health Across the Nation (SWAN). Annals of the New York Academy of Sciences, 828, 63-80.
6. Wright, V. J., Schwartzman, J. D., Itinoche, R., & Wittstein, J. (2024). The musculoskeletal syndrome of Menopause. Climacteric: The Journal of the International Menopause Society, 27(5), 466-472. https://doi.org/10.1080/13697137.2024.2380363
7. Frizzero, A., Vittadini, F., Gasparre, G., & Masiero, S. (2014). Impact of oestrogen deficiency and aging on tendon: Concise review. Muscles, Ligaments and Tendons Journal, 4(3), 324-328.
8. Chidi-Ogbolu, N.; Baar, K. (2019). Effect of estrogen on musculoskeletal performance and injury risk. Frontiers in Physiology, 9, 1834. https://doi.org/10.3389/fphys.2018.01834
9. Capel-Alcaraz, A.M., García-López, H., Castro-Sánchez, A.M., Fernández-Sánchez, M. & Lara-Palomo, I.C. (2023). The efficacy of strength exercises for reducing the symptoms of menopause: a systematic review. Journal of clinical medicine, 12(2), p.548.
10. Erdélyi, A., Pálfi, E., Tűű, L., Nas, K., Szűcs, Z., Török, M., Jakab, A. & Várbíró, (2023). The importance of nutrition in menopause and perimenopause—a review. Nutrients, 16(1), p.27.
11. Ganderton, C., Semciw, A., Cook, J. & Pizzari, T. (2016). The effect of female sex hormone supplementation on tendons in pre and postmenopausal women: a systematic review. Journal of musculoskeletal & neuronal interactions, 16(2), p.92.
12. Pettee Gabriel, K., Mason, J.M. & Sternfeld, B. (2015). Recent evidence exploring the associations between physical activity and menopausal symptoms in midlife women: perceived risks and possible health benefits. Women’s midlife health, 1, pp.1-28.
13. Baker, F.C., De Zambotti, M., Colrain, I.M. & Bei, B. (2018). Sleep problems during the menopausal transition: prevalence, impact, and management challenges. Nature and science of sleep, pp.73-95.
14. Sydney Pelvic Clinic. (2025). Menopause & the Musculoskeletal System. Retrieved from https://www.sydneypelvicclinic.com.au/menopause-and-the-musculoskeletal-system.


